Different types of injury
The basic principles
Sports injuries tend to be divided into two categories:
• soft tissue injuries (anything except bone)
• bony injury, which means either the bone is broken (fracture) or the bones are out of their normal alignment (dislocation).
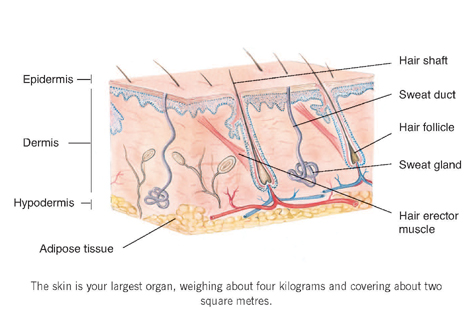
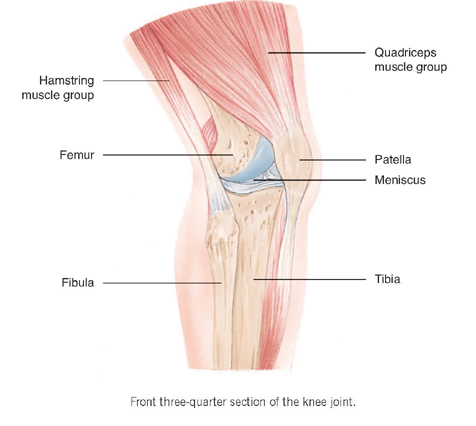
To understand how bone and soft tissue (which includes skin, muscle, tendon, cartilage and ligaments) can become involved in injury, you need to understand how these structures are related to one another anatomically. The easiest way to do this is to study a typical joint, which is where many sports injuries strike. Joints are vulnerable because, although they are flexible to allow movement, they are also liable to twists and sprains.
In many activities they take the brunt of the weight (for instance, the knees in skiing) and/or repetitive movement.
Every joint is different, but the general principles of how bone, cartilage, tendon and so on are related to one another remain the same.
Joints are where two bones meet. The ends of the bones that move against each other are protected by cartilage. The joint is enclosed within a joint capsule (made up of fibrous tissue) which, on the innermost surface, is lined by a membrane called the synovial membrane. This produces a viscous fluid (the synovial fluid) which lubricates the bone surfaces within the capsule.
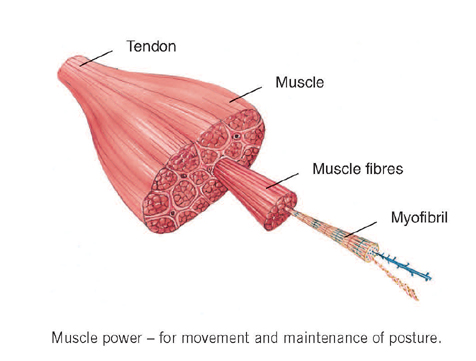
Muscles are attached to bones by tendons. Ligaments are supporting bands which connect one bone to the other, helping to hold the joint stable. Some joints have small thin bags called bursae (singular bursa), which add to the protection of the joint.

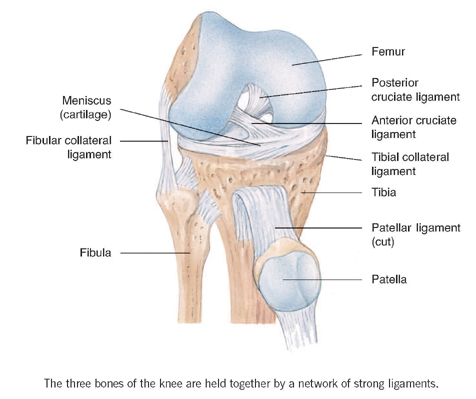
Actual joints are even more complex than this. For example, the knee joint is really a combination of three separate joints, and contains specially evolved tendons, ligaments and cartilage. Like any synovial joint, the ends of the knee bones are covered in white, smooth, articular cartilage. Second, the knee is unusual in having a pair of meniscus pads of shock-absorbing cartilage between the bones. It is these cartilages that get torn and sometimes need repair or replacement. A joint must be a complex structure to perform the wide range of movements demanded of it, but this also means that there is a lot of potential for things to go wrong.
Soft tissue injuries
Skin
Skin may be cut or burned (by friction or by the sun). Bear in mind that cuts and scratches sustained on the sports field are likely to become infected, so you should always wash them thoroughly before applying any dressing. Make sure that your tetanus immunisation is always up to date. There is a layer of fat under the skin and, if the blood vessels in this are damaged, blood leaks into the tissues and creates the characteristic purple colour of a bruise.
Swelling and pain are natural defence mechanisms by which the body immobilises the injured part. Tissue damage is usually accompanied by some bleeding and the injury often triggers the production of tissue fluid, resulting in a swelling. The damage and swollen tissue stimulate nerve endings in the area, causing pain. In addition the swelling makes the injured part feel stiff, preventing you from using it. This allows repair processes to begin work and stops you from inflicting any further damage.
The bleeding and tissue fluid make the area feel warm and reddened – in other words, it becomes inflamed. The main aim of treatment for soft tissue injury is to reduce this inflammation and so speed up your recovery.
Muscles
Injuries to muscles produce symptoms ranging from a ‘minor twinge’ when you move, which settles with time, to severe pain and fear brought on every time you do a particular exercise or movement. A pull or strain means that a few muscle fibres have been torn. A tear or rupture is more severe and is usually caused by a direct blow, such as a kick on the thigh. There may be bleeding, swelling and possibly a ‘dead leg’ caused by pressure on nerves. If you have severe symptoms of this kind, you should see a doctor on the day of the injury.
Putting an ice pack over the injured part will help relieve pain and swelling initially, then you need to apply a bandage and go to your local accident and emergency department if necessary.
Infection after muscle injury is very uncommon but sometimes cysts form inside the muscle if the bleeding has not settled adequately. These require medical treatment. A more common problem is shortening of the muscle as a result of formation of fibrous tissue which is less elastic than the muscle fibres themselves. This is why rehabilitation after any muscle injury must include stretching exercises to restore length and flexibility.
Thigh muscle injuries must be treated with particular respect or you may end up needing prolonged rest or surgical treatment. It’s not a good idea to massage a thigh muscle injury because, in some cases, this will increase the size of the blood clot within it. This may become hardened and calcified or even form a lump of abnormal bone.
Tendons, ligaments, cartilage and bursae
Tendons can become inflamed with overuse: a condition known as tendonitis. The tendon becomes swollen, red and tender to the touch and hurts when you move it. You’re most at risk of developing tendonitis if you perform one activity or movement regularly and intensely: runners get it in the Achilles’ tendon and racket players in the wrist, for example. As well as rest, treatment usually includes some method of changing the way the tendon moves: for example, wearing a heel pad in Achilles’ tendonitis. Treatment with non-steroidal analgesic drugs can also be helpful while the pain is severe and, if the problem does not clear up, you may need to have an injection of local anaesthetic and hydrocortisone into the covering of the tendon or possibly an operation to decompress the tendon.
Tendons can also be partially or completely torn. In a partial tear there is significant pain and discomfort and if the tear is complete you may be able to feel a gap in the tendon.
Ligaments can be stretched, leading to partial or complete tears. The word sprain is usually applied to minor tears of ligaments. These injuries result from twisting or wrenching of the affected joints. A complete tear will cause excessive pain, swelling, bruising or abnormal movement of the joint.
Bursae may become inflamed if they are constantly put under pressure and cartilage may be torn in more serious joint injuries. The knee joint contains the medial meniscus and the lateral meniscus – specially shaped cartilage at the top end of the tibia (the larger leg bone) – which can be torn by a fast, twisting action of the knee. This is a common football injury.
Always see a doctor for anything other than a minor injury, but first aid should follow what’s called the RICE principle.
TREATING SOFT TISSUE INJURIES:‘RICE’ PRINCIPLE
R = Relative rest
Some injuries may need complete rest because they are so serious but very often you will need only to limit your activities, cut back on training or change to another type of exercise. This is what is meant by relative rest and it allows you to maintain physical fitness while the injury heals.
I = Ice applied to the injured part
Ice reduces the amount of bleeding and bruising by cooling the blood vessels under the skin, making them constrict. It also has an anaesthetic effect, so it can relieve pain. When applying ice you must be careful not to burn the skin by direct application for too long. Either wrap the ice in a flannel or use a proper ice pack.
Ice is an important component of treatment of an acute injury, but don’t use an ice pack for longer than a period of 24 to 48 hours, during which you should apply it intermittently until the initial swelling goes down. Once the worst symptoms have subsided, usually after a week or so, there are many useful over-the-counter heat treatments for warming up the affected area. They are also worth using as part of your pre-match warm-up if you have a recurring injury.
C = Compressive bandaging
This is particularly effective in a limb injury. After you’ve applied an ice pack to the affected area several times for periods of 10 to 30 minutes, bandage it firmly if you can. This will also help to prevent further bleeding and swelling.
E = Elevation
Elevating the injured part allows the tissue fluid to drain away and will also help to reduce the size of the swelling and therefore relieve pain.
Bony injuries
Fractured bones and dislocated joints are potentially serious, and should be treated by a doctor in the accident and emergency department. Bony injury often causes much soft tissue injury, bleeding into muscle, swelling and pain. You may feel faint or pass out with shock, pain or blood loss.
In some fractures the skin is broken by the jagged ends of the broken bones, although sometimes all you can actually see is a puncture wound on the skin. When this happens, infection may get into the bone, so this must always be regarded as a particularly serious injury.
Joints may simply be dislocated, or be fractured and dislocated. A dislocated joint is usually very painful, looks odd and the limb affected hangs loosely because you can’t move it normally. All dislocations need urgent attention in accident and emergency because, the sooner they are put back, the better the outcome.

First aid for bony injuries
If the person is in considerable pain the quickest way to relieve it is to splint the injury. This may involve the use of a simple first aid splint or splinting an injured leg to the uninjured one or a damaged finger to its neighbour (buddy strapping). Injured arms can be made more comfortable with a sling or bandage. In such situations ask the person what feels most comfortable and try to immobilise the limb in that position. Do not let the person eat or drink in case he or she needs an anaesthetic later.
Once in accident and emergency, an X-ray will be taken of the injury. Some fractures can be ‘reduced’ (realigned) using local anaesthetic techniques and sedation without an operation. Other fractures require ‘internal fixation’ – that is, they need metal plates and screws to hold the bones in place while healing takes place. An operation is required. A general anaesthetic cannot be given until FOUR hours after the last drink, and SIX hours after the last meal, because vomiting and choking under an anaesthetic are dangerous.
Most reduced fractures are held with a plaster cast, to immobilise the limb. Expect to wear the cast for about six weeks, but the precise timing varies from one person to another.
Skin injuries and problems
Blisters
These are caused by shearing forces, such as the movement of the foot inside a training shoe, which is one reason why you should always wear well-fitting shoes and thick socks. When possible, smearing the skin with petroleum jelly may prevent friction. If you do get a blister, puncture it with a sterile needle, then cover it with a dressing to prevent further damage.
Abrasions
Wash broken and grazed skin with soap and water or an antiseptic agent to remove dirt, then cover it with a sterile dressing.
Cuts and lacerations
A cut is an injury produced by a sharp edge such as broken glass or the blade of a knife, whereas a laceration is a ragged cut usually caused by a blunt object. Cover the injury with a sterile dressing and apply pressure to stop bleeding. If the cut or laceration is minor you can wash it with soap and water, but more serious cuts or lacerations and those that may contain foreign bodies or that fail to stop bleeding need to be seen by a doctor.
Bruises
These are caused by bleeding under the skin; very extensive bruises are called haematomas. A haematoma is a collection of blood within a space, for example, in the quadriceps muscle on the thigh or in the soft tissue around the eye (black eye), or under the skin of the shin bone. Haematomas can also occur within joints and in the chest, abdominal or skull cavities. Minor bruises require little treatment other than cooling. Haematomas may require medical attention and it’s wise to go to the hospital accident and emergency department. Haematomas usually occur in the large muscle groups, particularly quadriceps muscle of the thigh. Sometimes a haematoma can be very large indeed and it may be necessary to accelerate healing by aspirating it under aseptic conditions. This usually involves having a local anaesthetic so that a large-bore needle can be inserted to draw out the blood into a syringe.
Burns
Other than in motor sport, burns are usually caused by friction rather than physical heat. Wrestlers and judo practitioners may get mat burns (grazes) while grass burns are associated with playing on synthetic turf. Burns may also be caused by one body part rubbing repeatedly against another (such as inner thighs in runners) or clothing (nipple burn in women runners). Covering the area with petroleum jelly can prevent this.
Other burns should be immediately cooled with tap water or an ice pack and usually no other treatment will be necessary.
Fungal infections
The moist environment created when you sweat for long periods encourages fungal infections such as ‘athlete’s foot’ or ‘jock itch’. Communal showers and swimming pools are often breeding grounds for the organisms leading to these infections. Personal hygiene is also important to discourage infection.
Fungal infections cause an irritating itch between the toes or in the groin crease. You pick them up through direct contact with floors, shower rooms and other moist surfaces which actually harbour the infection. Using the same towel all week or sharing towels with other people may be a factor too.
If possible you should have two or even three sets of training gear so that one is always freshly washed. If you are using only one set of training clothes wash them as regularly as possible, at least twice a week, and leave them to dry overnight. If you’re involved with managing children and teenagers, try to arrange for training clothes or team clothes to be laundered on a regular basis, so that they are fresh at least once a week. The importance of fresh kit cannot be over-emphasised.
To prevent athlete’s foot, make a point of washing your feet quickly in warm water, without soaking them, at least once a day and certainly after every training session. Dry them gently and wait several minutes before putting on your socks which should also be changed daily. By all means use talcum powder if you want to once your feet are dry but remember that it is no substitute for proper drying, especially between the toes. Nylon socks actually increase sweating so opt for wool or cotton with a minimum of synthetic fibres.
You can buy antifungal preparations to treat athlete’s foot or groin from the chemist without a prescription. If there is no improvement after two weeks consult your doctor. Spread a towel to stand on after showering to avoid passing on the infection to other people, and don’t use the towel for anything else.
Do not walk with bare feet on surfaces used by others. Use a separate towel to dry the groin creases and keep your underwear clean and fresh.
Verrucas and corns
You are vulnerable to getting footwarts (verrucas) if you take part in activities with bare feet such as swimming, karate or judo. A verruca always occurs in the sole of the foot and feels as though you are walking on a small pebble. Specialist treatment from either a doctor or chiropodist is required.
A corn is a thickening of normal skin resulting from friction from shoes, usually at the pressure points. Treat it with lanolin and then abrade it with an emery board (a cardboard nail file).
Facial injuries
Our psychological and social well-being depends very much on how we look and having a heavily scarred face can be stigmatising. You need to protect important areas such as your eyes, ears, nose and mouth from any injury.
Cauliflower ear
This is common in combat sports such as boxing and wrestling and in contact sports such as rugby. It results from a blow to the area which causes bleeding under the skin of the ear. Apply an ice pack for first aid, but all such injuries should be seen as soon as possible by the club doctor, who will remove the haematoma and prevent its recurrence by applying pressure dressing or prescribing appropriate medication.
Broken nose
This often follows a hard blow and can occur with or without deformity of the nose. Usually, when nasal cartilages dislocate from the bone they cause deformity, although in some cases the bone itself actually breaks. If there is a break in the skin or obvious deformity, you need to get to hospital as soon as possible. The nose can often be pushed back into position under local anaesthetic, and will look normal afterwards. In sports where a broken nose is a recurrent problem, these injuries produce the classic picture of the ‘boxer’s nose’.
Broken cheekbone
You can feel this bone just in front of your ear and where it passes across your face to your nose. It gives the middle part of your face its fullness. When it’s broken, your face on that side may look flattened and there may be blood in the white of the eye. You may find it difficult to open your mouth so you have to talk through your teeth. An operation is necessary to correct the deformity so you must go to accident and emergency.
Fractures of the jaw
The symptoms include pain in the jaw and you may have trouble talking or gritting your teeth and notice blood in your saliva. You need to get to hospital straightaway as all fractures of the jaw need medical attention. The jaw may have to be ‘wired’ – that is, fixed in position with the mouth closed – to allow healing. Remember to wear a gumshield in contact and combat sports because this prevents many injuries.
Dental injuries
These are almost 100 per cent preventable simply by wearing a properly custom-built gumshield for any high-risk sports. Make sure that children’s gumshields are renewed regularly as they grow. Ask your dentist about this service.
If the tooth is still attached to the gum, try to return it to its original position by gentle pressure. If it has been completely dislodged wash it and try to push it back into its socket. If this is not possible, put it inside its owner’s mouth between the gum and lip. Once this has been done, the person should go straight to a dentist. If a tooth is replaced within the hour it may be saved.
DO NOT PLACE LOOSE TEETH INTO THE MOUTH OF ANYONE WHO IS NOT FULLY CONSCIOUS.
Eye injuries
Eye injuries are very common, and almost 90 per cent of them are preventable. About one-third are serious enough to require hospital admission for treatment. Unfortunately such injuries predominantly affect young men under 25, including a very large number of children, half of whom will suffer permanent loss of their field of vision or of the ability to focus properly.
High-risk activities include any sport involving missiles (balls, shuttlecocks) or rackets or sticks, combat sports such as karate, boxing and contact sports such as football and rugby.
The most common serious injury is caused by a direct blow to the eye by a fist or a ball. This compresses the eyeball into its socket and leads to potentially serious complications throughout the eye, including rupture of the eyeball. The most visible sign is a black eye, caused by bruising, but this in itself is not harmful. It may, however, make examination of the eye more difficult. Otherwise, the cornea may be scratched, the iris torn or the lens dislocated.
If you are in intense pain and feel unwell and sick, this is a sign that the pressure within the eye is increasing (as a result of bleeding) and urgent medical help is needed.
Other mishaps include torn eyelids, scratched corneas, grit or dust in the eye. Wearing goggles prevents the cornea becoming inflamed from contact with chlorine in the swimming pool, and the right protection can prevent your eyes becoming raw after too much exposure to ultraviolet radiation, as in snow-blindness in skiers and mountaineers.
All eye injuries should be quickly assessed on the spot. If there is any pain, swelling, change in vision or change in the shape of the pupil, get medical attention urgently. Simple problems like corneal scratches and grit in the eye can be dealt with by the A&E staff; more serious problems will receive the attention of the eye surgeon.
Shoulder, arm and hand injuries
Dislocated shoulder
This is caused by a fall on to the outstretched hand. The shoulder looks deformed, square in appearance, and the arm appears too long. The injured person supports the arm with his other hand. Diagnosis is confirmed by X-ray, which will also reveal any fractures near the dislocation.
Treatment:
• Reduction of the dislocation (putting it back) should take place in hospital. This can be done under sedation, but often a general anaesthetic is needed.
• Healing of the soft tissues may take 2–4 weeks. After this the shoulder may be exercised, but return to full sport, especially contact sports, should be delayed for 2–3 months.
• In some cases, actual shoulder dislocation, or the feeling that the joint may dislocate, may become a recurrent problem. This can have serious consequences for the patient’s sporting prospects, and needs to be assessed by an orthopaedic surgeon. The joint may be repaired under general anaesthetic.

Broken collar bone
This is caused by a fall on the outstretched hand and is especially common in young people and children. There is usually obvious deformity and the skin may be broken. The injured person supports the damaged arm with his other hand.
Treatment:
• This injury is managed in hospital, usually with the application of a sling or braces.
Acromioclavicular joint damage
There is a small joint between the collar bone and the shoulder blade, at the tip of the shoulder. It can be damaged during contact sports, as a result of a fall on to the point of the shoulder or the outstretched arm. There is tenderness and swelling over the affected area and sometimes a step can be seen between the end of the collar bone and the shoulder itself.
Treatment:
• The injury should be examined in the accident and emergency department. Usually, the arm is placed in a broad sling.
• Once the pain subsides, the arm and shoulder can be exercised with pendular movements.
• In more serious cases, the joint may need repair with screws, which are removed after six weeks.
Rotator cuff lesions
This is the medical term to describe a group of soft tissue problems around the joint capsule of the shoulder. Sports that require repetitive overarm movement – such as bowling a cricket ball, swimming, serving a tennis ball – can lead to irritation and inflammation of the tendons and bursa around the shoulder. Overarm movements become painful, which can badly affect sporting performance. Acute shoulder tendonitis causes rapid-onset pain on lifting the arm away from the body. Rotating the arm may also be painful. Chronic shoulder tendonitis tends to affect weekend sportsmen. The pain develops gradually over several weeks. The shoulder may not be tender, but it is still painful to make an arc with the arm.
Treatment:
• In mild cases, resting the arm in a broad sling for a few days,
plus regular anti-inflammatory medication, should suffice.
• In more severe cases, injections of local anaesthetic mixed with steroids into the shoulder joint may be helpful.
• GPs may treat mild cases, but more severe cases are referred to hospital specialists.
Tennis elbow
Pain on the outer part of the elbow, especially when you’re gripping a racket, is called tennis elbow and the area over your outer elbow may also feel tender. This is an overuse injury common in racket sports but can be caused by any repetitive movement.
Treatment:
• Apply ice packs and take several days’ rest. Avoid moving your arm in such a way that it hurts.
• Use a supportive bandage or strapping for the muscles of the upper forearm.
• Take simple pain-killers such as aspirin or paracetemol (if you can tolerate them).
• Consider changing the size of your racket handle.
• If you are still in pain after a few days, see your doctor who may give you local anaesthetic and steroid injections.
Golfer’s elbow
This affects the inside of the elbow and is caused by forceful stretching of the ligaments and muscles on that side. It is common in golfers and racket players.
Treatment:
As for tennis elbow.

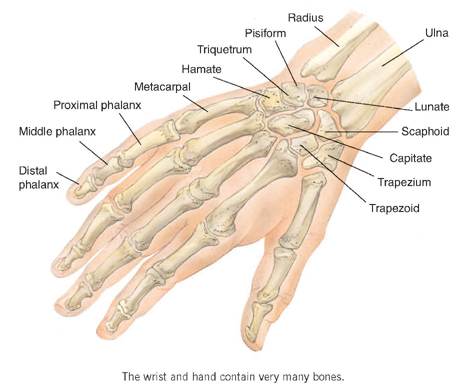
Wrist strain
This is caused by repetitive or unaccustomed use of the wrist and is common in racket sports. There is pain on the back of the wrist and thumb with a crunching sensation as the tendons move.
Treatment:
• Apply the RICE principle.
• Anti-inflammatory drugs are often helpful, provided you don’t have any troublesome side effects.
• Splinting may ease the pain.
• Avoid repeating the movements that produce the symptoms.
• If you injure your wrist in a fall, always get it checked out by a doctor to rule out a hard-to-detect fracture of a small wrist bone called the scaphoid bone. If the scaphoid is fractured, there will be tenderness in the area between the wrist and base of the thumb, and pain when the thumb is pulled backwards. Scaphoid injuries are diagnosed by means of an X-ray, and your arm will be placed in a plaster cast for six to twelve weeks.
Finger and thumb injuries
Strains, fractures and dislocations are common; strains or tears to the ligaments at the base of the thumb are especially important. Such injuries cause severe pain.
Treatment:
• Thumb injuries should always be treated in hospital because you can’t grip if you can’t use your thumb, whereas finger sprains, while very painful, do not usually require medical advice.
• Fingers can get dislocated in contact sports such as rugby. If the skin is undamaged, the dislocation can be reduced at the time by pulling the finger straight, allowing the joint to slip back into position. Try this only once and if you fail take the person to hospital. If it works, strap the injured finger to the one next to it (buddy strapping) to relieve the pain.
• Finger fractures should also be seen in A&E. Often immobilisation by buddy strapping is all that is required; however, more severe fractures may need to be held in place with a wire, which is inserted under general anaesthetic.
Lower limb injuries
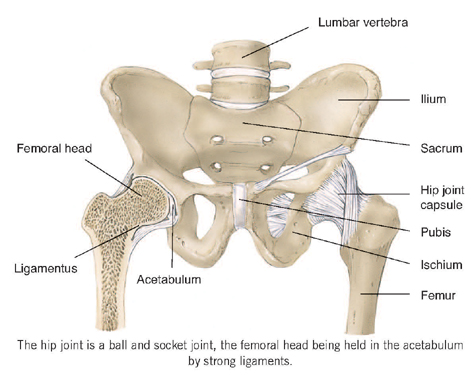
Clicking hip
You may develop this if you do a lot of stretching exercises: as you stand with your legs apart and stretch you hear a loud clunk which isn’t usually painful. A clicking hip is fairly common and is caused by a tight band of muscle or tendon sliding over the outer part of the hip joint. If you do get pain with it, see your doctor.
Adductor muscle tears
The muscles on the inside of the thigh can be torn during over-enthusiastic stretching exercises or when making a football tackle. Sometimes a splinter of bone is pulled off as the muscle tears. The injury is very painful, particularly on stretching or whenever the muscle is tensed.
Treatment:
• Apply the RICE principle as quickly as possible
• Once the initial pain has passed, make an effort to use the muscle gently in stretching movements but always within the limits of pain.
• Take soluble aspirin or ibuprofen at the time of the injury and four-hourly afterwards for the first day to ease the pain.
Groin pain
This type of injury mostly affects people taking part in soccer, hand-ball, ice hockey, skiing, athletics and horse riding. Groin pain can be the result of an overstretch injury or inflammation of tendons in the thigh and abdomen. The arrangement of muscles in this region is complex, and many muscles are vulnerable to overuse pain. Groin pain may also be caused by unstable pelvic bones.
You normally notice a gradual ache in the groin which becomes worse after activity. It may cause difficulties with kicking a ball or hurt when you cough or get out of bed, for example.
Treatment:
• Relative rest.
• Take an analgesic (pain-killer) such as soluble aspirin.
• Begin gentle remobilisation after several days.
• Physiotherapy exercises.
• If the problems persist, you may require surgery to repair a tear in the muscle of the lower abdominal wall or even a small early hernia.
Thigh injuries
The thigh muscles (the quadriceps at the front and the hamstrings at the back) may get bruised, usually following a direct blow which causes a sudden pain followed by a deep aching and sometimes obvious swelling.
Treatment:
• Use the RICE principle (see page 65) and, if necessary, spend a day or two in bed to let the swelling settle.
• Never massage a thigh injury because this may produce complications (including abnormal bone formation) and delay healing.
• Carefully limit all activities for the few days after injury to prevent complications.
• See a doctor in the accident and emergency department within 24 hours of the injury if you have a lot of swelling and severe pain.
Muscle strains and ruptures
A direct severe blow is the usual cause: you may experience the feeling of a ‘dead leg’, tenderness at the site of the injury and sometimes you may be able to feel a gap in the muscle. It hurts when you try to tense the muscle. Alternatively you may have overused one or more muscles in the thighs or abdomen, making it painful to move in certain ways.
Muscle strains causing pain in the pubic region (adductor longus muscle), the inner thigh (iliopsoas), the front of the thigh (quadriceps) and the upper or lower thigh (hamstrings) are all relatively common.
Treatment:
• Apply the RICE principle.
• Take simple analgesic drugs.
• Start gentle exercises once the pain has settled.
• If the symptoms haven’t gone after two or three days see a doctor.
You may get repeated muscle strains because of the formation of scar tissue which is not as flexible as normal muscle. With all muscle injuries, adequate rest and gradual return to training are critical, because a quick return may cause recurrence.
Make sure you don’t overtrain and, if your problem is severe, you may need to alter your activities, so that less strain is placed on the same muscle.

The knee
Runner’s knee
This is pain in the region of the knee cap caused when it repeatedly rubs against the lower end of the thigh bone. Looked at through an arthroscope (a small viewing device inserted under general anaesthetic), the knee-cap cartilage may be abnormal, but even if it is not you may still be in considerable pain. Women are more prone to this problem than men. The cause is thought to be a slight misplacement of the knee joint and quadriceps muscle, or a slight deformity in the way the leg moves, which comes to light only with training.
You may feel pain and clicking behind the knee cap after training and/or sitting for a long time. Going down stairs is also painful and you may see a small swelling.
Treatment:
• Apply the RICE principle.
• Strengthen the quadriceps muscle: sit upright with your knees bent at 90 degrees, then straighten the leg. A light weight may be strapped to the foot for more intense exercise.
• Consider a carefully balanced muscle retraining programme.
• Avoid sitting still with the knee bent for long periods; keep the knee mobile.
• If none of this helps, you may need to see a specialist who will decide whether you need surgery. Arthroscopy is a telescopic exam ination of the knee joint during which therapeutic surgery can be performed; other forms of surgery involve exposing the knee cap and either making the under-surface smoother or realigning the knee cap so that it no longer rubs against the lower end of the thigh bone. The attraction of arthroscopy is that you can get back to your normal activities relatively quickly afterwards.
Knee ligament injuries
The knee has four main ligaments: two inside the joint (cruciate ligaments) and two on either side of the knee (collateral ligaments). Most injuries are the result of twisting movements (such as in a football tackle) or a direct blow. Minor sprains may cause tenderness in the inside or outside of the knee joint. In major injuries the knee will ‘bend’ the wrong way. Paradoxically, complete tears of ligaments are less painful than partial tears. Your knee may feel unstable when walking or running, especially when changing direction.
Treatment:
• Use the RICE regimen (see page 65) for first aid.
• Have the knee examined by a doctor if possible because you may need surgery to remove blood from the joint or to repair the ligaments if it’s unstable.
• After surgery, the knee will be placed in a plaster cast for four to six weeks, then you will follow an exercise regimen involving increasingly rapid running movements.
Torn cartilage (meniscus injury)
The meniscus cartilages are two C-shaped wedges between the femoral (thigh bone) and tibial (shin bone) surfaces of the knee joint. They are attached to the tibia at its upper end and are thought to act as shock absorbers and to allow the even spreading of joint fluid. When torn they can become loose inside the joint and interfere with its movements.
Soccer alone accounts for almost 70 per cent of meniscus injuries. The knee suddenly gives way or locks and can’t be immediately straightened.
Treatment:
• The RICE regimen should be your first recourse.
• If your knee locks, swells, is persistently painful or gives way, you need a medical opinion. You will have an arthroscopy (see page 81) and the torn cartilage will either be repaired or, if the tear is too extensive, it may be partially or completely removed.
• No artificial cartilages are used in this country at present.
Lower leg injuries
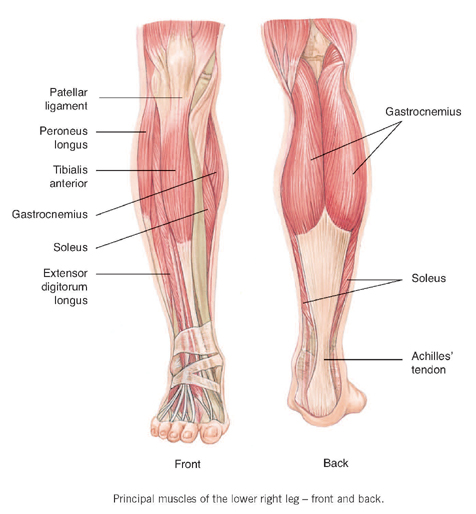
The two bones of the lower leg are the tibia which bears the body weight and the fibula, the strut-like bone to which the three groups of lower leg muscles are attached. The two in the calf are the gastrocnemius and soleus, which form a tendon that is inserted into the heel bone, the Achilles’ tendon. These muscles provide the propulsive force for actions such as sprinting and jumping.
At the front of the leg another group of muscles pulls the ankle upwards – you can feel them tense and relax as you move your foot up and down. Combined muscle action allows you to turn the foot outwards or inwards.
Stress fractures
These are overuse injuries. A stress fracture is a crack in the bone caused by repeatedly striking the foot on the ground and can occur in many sports including football and long distance running. (They usually affect the lower limb but can also occur in the bones of the spine and even in the ribs in one golfer!) The classic symptom is pain provoked by activity and the area over the fracture will be tender.
A stress fracture can usually be diagnosed by an X-ray two or three weeks later when signs of bone healing become visible or at an earlier stage by means of a bone scan.
Treatment:
• If a fracture is in a weight-bearing bone then rest is essential; otherwise just reducing your level of activity for about six to eight weeks will usually allow it to heal.
• Allow at least a further four weeks before starting graduated training again and be prepared to slow the pace if exercise triggers any pain.
Shin splints
This condition is usually the result of repetitive movements which lead to inflammation of the tendons and muscle attached to the shin, but symptoms can also be the result of a stress fracture or swelling of the muscle. You feel pain down the front of the leg, usually in the lower half from the mid-point of the tibia bone down to the ankle. It gradually increases and eventually you feel pain both during and after running and even while walking.
Your calf may be tight and you may get cramps or occasionally numbness of the foot. Novices training on hard roads or who are in poor physical condition are particularly susceptible.
Treatment:
• Apply the RICE principle.
• Reduce your training programme so that it isn’t painful.
• Always exercise on a soft surface like grass.
• Wear good quality absorbent footwear.
• If you suspect your running style may be faulty, get advice from an experienced coach.
• If all these measures fail seek medical advice.
Tibial compartment syndrome
This is a form of shin splint that affects the muscles on the front of the lower leg. They lie between two bones, the tibia and fibula, and they are strongly encased in a tough fibrous tissue called fascia.
Sometimes after strenuous activity or even a direct injury this part of your leg swells, compressing the artery which is its blood supply. Symptoms are severe pain on the front of your leg and sometimes you may feel a numbness between the first and second toes.
Treatment:
• Stop your exercise.
• Elevate the limb and apply the RICE regimen.
• See your doctor because you may need surgery to decompress the leg.
• The condition can also occur in untrained people in a more chronic form. This doesn’t need urgent treatment and usually changing your training programme so as to stop the pain works well but, if not, you may need surgery.
Achilles’ tendon
The Achilles’ tendon is a potential weak spot in top-class athletes who do a lot of road running, and middle-aged and older exercisers. The most common problems are rupture and tendonitis.
• Achilles’ tendon rupture:
Older exercisers (middle age onwards) are most vulnerable, but this problem can affect young people, especially after a blow to the tendon. The tendon becomes very painful and it may be difficult to stand. Gentle examination will reveal a gap which can be felt in the tendon.
Treatment:
• This must be carried out in hospital. Surgery is one option and, if it is necessary, it must be performed as soon as possible. You will have a plaster cast on your leg for about six weeks afterwards.
• An alternative is simply to put the leg in a cast for a longer period (eight weeks) followed by a longer programme of rehabilitation.
• While the injury is healing, you’ll have to walk with your heel raised to relax the tendon, and you’ll be given exercises to stretch and strengthen your calf muscles.
• Whichever form of treatment you are given, the outcome will be much the same after six to twelve months. The tendon will be as strong as before and you should be able to use your leg normally. One man retained a world karate championship title despite sustaining a traumatic rupture of the Achilles’ tendon during training.
• Tendonitis:
This is inflammation of the covering of the Achilles’ tendon. It usually starts with a vague ache which gets progressively worse until the whole tendon becomes swollen and very tender to touch; you may also feel crackling as your foot moves up and down.
Treatment:
• Rest is essential after you’ve applied the RICE regimen.
• Wearing a heel raise of one to two centimetres inside your shoe can relieve symptoms.
• You may require physiotherapy.
• Anti-inflammatory drugs can help.
• In chronic cases surgical treatment is necessary.
• When the symptoms are subsiding, you should avoid stressing the tendon. Run or walk on grass rather than hard surfaces when possible, avoiding hills, and continue to wear the heel raise.
Calf strain
This can be caused by overuse or a direct blow although there may be no obvious cause in an older person. Your calf will be painful and swollen and you may be able to feel a gap in the muscle.
Treatment:
• Apply the RICE principle at once and continue with it for 48 hours.
• Begin gentle stretching exercises within the limits of pain after
48 hours.
• Consult your doctor if you can feel a gap in the muscle
Cramp
This mostly affects the legs but you can get it in any group of muscles. It is a painful and persistent spasm of a muscle caused by over-contraction of a muscle or a group of muscles, sometimes because you are dehydrated or cold. Although the exact cause of cramp isn’t fully understood, it may be related to the accumulation of waste products within the muscle. As well as being very painful, the muscle is tightly contracted.
Treatment:
• Stop whatever activity you were doing.
• If the cramp is in your calf, gently stretch the muscle by pushing the sole of the foot upwards while straightening the leg. This often allows the muscle to relax.
• Once the cramped muscle is released, you need to rest.
Foot problems and injuries
Blisters
Blisters are caused by shearing forces often associated with poor footwear or wrinkled socks.
Treatment:
• Prick the blister with a sterile needle.
• Drain the fluid.
• Cover the blister with tape or a dressing to protect it and enable you to carry on exercising.
Jogger’s toe
This is common in people who do long-distance running and can be very painful. It appears as a bruise under the toenail and is caused by ill-fitting training shoes.
Treatment:
• See your doctor, who will probably pierce the nail and drain the blood.
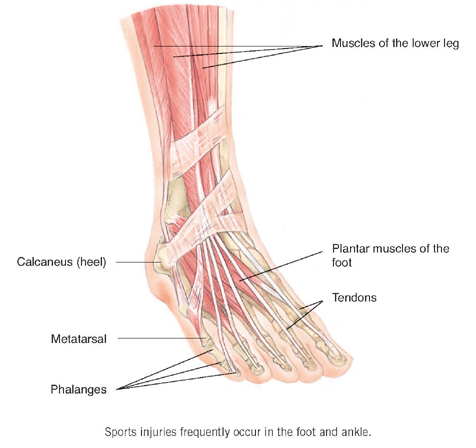
Heel spur syndrome (plantar fasciitis, policeman’s heel)
Your heel and the arch of your foot will be painful and may be extremely tender to touch. An X-ray will reveal the heel spur, which is often associated with a strained arch or the so-called policemen’s heel. Whether the spur itself is significant remains controversial. The cause of plantar fasciitis is poor instep support and repetitive activities (such as walking the beat). These are both related to unsuitable or inadequate footwear.
Treatment: When the pain is severe:
• Apply the RICE principle over 48 hours.
• Work out what is causing the problem so you can eliminate whatever it is.
• Wear a heel pad in your shoe.
• Do stretching exercises to stretch the calf muscles and the Achilles’ tendon.
• If there is no improvement, see a doctor. Injecting the heel with local anaesthetic and steroid can cure the condition.
KEY POINTS
♦ Injuries may be to the soft tissues (skin, muscles, tendons, nerves, ligaments) or to bone
♦ Apply the RICE principle when treating soft tissue injuries
♦ Cuts, lacerations, burns, infections and suspected broken bones may require medical treatment
♦ Eye and teeth injuries may be prevented in almost 90 to 100 per cent of cases
♦ Avoid using non steroidal anti-inflammatories (NSAIDs) in muscle injuries. They may delay healing
♦ Specialist treatment with platelet rich plasma may accelerate healing
